Mpox is killing again. It didn’t have to be this way.
Missteps by the World Health Organization, a vaccine manufacturer and an African country led to another health emergency, experts say.
Mpox is back. More than 900 people, mostly African children, have died this year and public health officials say the new variant inflicting that toll could arrive in the U.S. at any time.
There’s a lot of blame to go around.
It was only two years ago that mpox, previously known as monkeypox, arrived in the U.S. and began spreading. U.S. authorities contained it with a vaccination campaign targeted at those most at risk, men who have sex with men. But no vaccines got to Africa, where the disease is endemic in some countries, making it easier for the new variant to emerge.
That proved costly, according to public health officials, who say it’s another demonstration of why pandemic preparedness requires global cooperation. Authorities in Europe and Asia have detected infections of the new variant in people traveling from Africa and fear it could spread further. The outbreak that started in 2022 reached more than 100 countries and infected at least 100,000 people.
“There’s plenty of blame to go around in terms of what could be done and how things could be done differently. But every single one of us needs to be asking that question,” said Maria Van Kerkhove, the World Health Organization’s incident manager for the global mpox response.
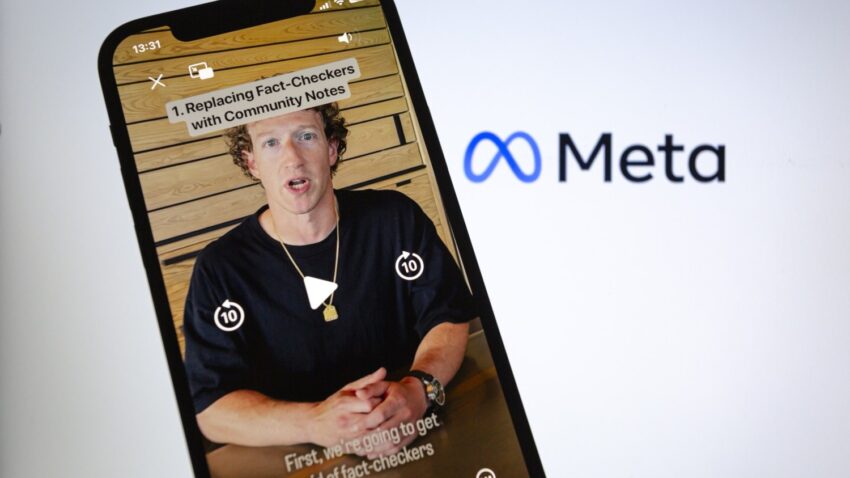
Leaders of the Democratic Republic of the Congo, the epicenter of this year’s outbreak, until recently refused to accept donated vaccines. The WHO and the manufacturer of the mpox vaccine are pointing fingers at each other for the delay in reassuring the DRC and other developing countries that the shot is safe and effective. The WHO signed off last month.
The DRC health minister and the coordinator of its response committee did not respond to repeated requests for an interview, but a leading African health official said it was part of the legacy of mistrust between Africa and the West that the WHO, an arm of the United Nations, could have done more to relieve.
More than a dozen African countries have reported more than 38,000 suspected mpox cases since the beginning of the year, most of them in the DRC, according to the Africa Centers for Disease Prevention and Control. The disease causes a gruesome, painful rash and in vulnerable people can be deadly.
The WHO and Africa CDC declared the outbreak an international public health emergency in August. The variant seems to be more transmissible and deadlier than the one that caused thousands of U.S. cases in 2022 and 2023. The earlier variant continues to spread in the U.S. at low levels.
Paul Chaplin, the CEO of Bavarian Nordic, the Danish company that produces the vaccine, said the company asked the WHO for approval in March 2023. That would have allowed countries that hadn’t yet approved it on their own, such as the DRC, to import it.
But Van Kerkhove said the WHO did not receive all the needed information from Bavarian Nordic until late August. Chaplin said nearly a year had passed before the WHO asked for the additional details.
Van Kerhove rejected that assertion. “We have been communicating with Bavarian Nordic and other manufacturers in 2022, in 2023 and in 2024, and we didn’t receive the full information [to approve its shot], so we can’t assess the package of materials until we have that,” she said.
Dr. Jean Kaseya, director-general of Africa CDC, said DRC officials were waiting for the WHO’s assurance that the vaccine was safe and effective.
But the DRC also shares blame, said Larry Gostin, director of the O’Neill Institute for National and Global Health Law at Georgetown University, who speaks frequently to the White House and the WHO about global health issues.
“[The United States] has been for years now trying to donate doses to the DRC, and they weren’t accepted,” he said, citing foot-dragging on approvals by the Congolese health authorities and the WHO.
Challenged by armed conflict in some parts of the vast country — more than five times the size of California — multiple health crises and poverty, despite mineral wealth, Congolese authorities did not make fighting mpox a priority, said one global health official granted anonymity to speak candidly about a sensitive issue.
“This is a story of inequity and neglect, but it’s also a story of regulatory failures,” said Gostin.
A new variant
Mpox has afflicted the DRC for decades, but cases there and in the neighboring region have risen 300 percent this year compared to a year ago, according to Africa CDC.
Local and international experts cite a new variant called clade 1b. It was first detected a year ago in the Kamituga Health Zone, a densely populated gold mining region in the country’s remote east. Many of the confirmed cases were among female sex workers, indicating the virus was transmitted through sexual contact.
Clade 1b has now spread to the eastern DRC provinces of North and South Kivu, which have been rocked by conflict between the Congolese army and the M23 rebel group, leading to the displacement of more than 1.3 million people across the region. Warring parties have killed, kidnapped and threatened health workers, looted health supplies, and damaged and vandalized health centers, according to a coalition of health and human rights groups.
The number of mpox cases in displaced people living in camps in Goma, the capital of the North Kivu province, is increasing. “We’re watching this like milk on the stove,” said Sylvie Jonckheere, an adviser in emerging infectious diseases for Doctors Without Borders, who recently returned from the region. The high rate of rape near the camps makes the situation critical, according to Doctors Without Borders.
Congolese authorities have also reported cases in the country’s capital, Kinshasa, a crowded city of more than 17 million people, triggering concerns that the outbreak could expand rapidly.
Most of the cases and deaths are now in children under 15, who get the virus from close contact with family and from sharing bedding. Malnutrition, combined with a lack of access to care, makes them vulnerable.
But vaccines do work against all variants, based on the data available so far.
Last month, the DRC received about 250,000 doses of Jynneos, which U.S. and European authorities deployed to quell the 2022-2023 outbreak. Most of the donated shots came from the European Union. The U.S. contributed 50,000. Some 1,600 people were vaccinated with the first dose since the immunization campaign started on Oct. 5.
And more are on the way. Western countries, Japan and two mpox vaccine manufacturers have pledged some 5 million vaccine doses to the affected African countries, according to a tracker run by an affiliate of the Council on Foreign Relations think tank.
Japan has committed the most: 3 million doses of its domestically developed LC-16 vaccine, which is approved for children, followed by the U.S. with just over 1 million Jynneos doses. President Joe Biden has also pledged $500 million to help contain the outbreak.
Africa CDC estimates that 10 million doses and $600 million are needed to achieve that goal. It has already received financial pledges of more than $800 million, the institution’s leader, Kaseya, said in late September.
India, Sweden and Thailand have together reported a handful of cases associated with travel.
There has been no confirmed case of the clade 1b variant in the U.S. yet.
But Dr. Ashish Jha, dean of the School of Public Health at Brown University and the former White House Covid-19 response coordinator, said it’s only a matter of time until that happens. He expects mortality to be very low if cases are in mostly healthy young men, as happened during the 2022-2023 outbreak. Even so, it could be dangerous for people with HIV or who are immunocompromised, he said.
The CDC has urged men who have sex with men and people traveling to the affected countries to get vaccinated. The federal government has also made testing widely available and has told health care providers what to look for in this outbreak, CDC officials said.
Laying blame
Mpox used to be called monkeypox — stemming from its discovery in captive research monkeys in Denmark in 1958.
The WHO, which has the authority to name new diseases and rename existing ones, decided to change it to mpox in late 2022 to avoid it being associated with a racist trope.
The disease is endemic in central and west Africa, where animals carry the virus that causes the disease, but mpox only received global attention when it spread around the world for the first time in 2022.
The WHO declared that the outbreak was over in May 2023, as the number of cases declined. The committee of experts advising the WHO on it did note the “continued lack of effective countermeasures in the African countries, where mpox occurs regularly,” but most national and global health officials moved on.
So did the WHO, according to Bavarian Nordic’s Chaplin. “The urgency maybe was no longer there, maybe they were higher priorities with the WHO,” he said. “We didn’t have any interaction with them until earlier this year.”
Stephanie Psaki, the White House global health security coordinator, said competing priorities led to the WHO not endorsing the mpox vaccine earlier.
“As the emergency of the 2022 mpox outbreak waned, there were other products that were a higher priority, and I think that probably was the right call in 2023,” she said at a Center for Global Development event in September, referring to the WHO process for endorsing mpox vaccines.
The O’Neill Institute’s Gostin and others also point fingers at Bavarian Nordic for not producing more and cheaper vaccines for the countries where mpox is endemic.
“They have a lot of blame because now they’re saying they can ramp up to millions of new doses, but they’ve never done that before; they’ve never made it accessible and affordable in Africa, and they’ve never shared their technology with other manufacturers,” Gostin said.
Chaplin said his company is better positioned now to produce more doses than in 2022 when it renovated one production facility and had to get another one approved by regulators. But he defended the shot’s price, which the WHO put at between $50 and $75 per dose, though Chaplin declined to confirm the price. UNICEF said in late September it had negotiated a price of up to $65 per dose, which it called the lowest on the market.
“We’re not selling sufficient volume at a higher price to allow us to deliver at a much lower price,” Chaplin said.
As for the DRC’s refusal to accept vaccines before the outbreak had spread, Africa CDC’s Kaseya said African officials were wary of a shot that had not received WHO endorsement and that some suggested should also undergo clinical trials in Africa.
Another factor, he said, was a lack of trust among many African countries in the West, caused by the reluctance of the U.S. and Europe to share shots with them during the Covid-19 pandemic and the first mpox outbreak.
“The question was: ‘Why now? What is motivating you?’” Kaseya said.
What's Your Reaction?